When it comes to eating disorders what treatments work?
“We live in a dieting culture so it’s easy to be triggered. Letting go of the diet mentality will be an ongoing practice—remember to be patient with yourself.“
—Evelyn Tribole and Elyse Resch
Eating disorders are on the rise – and even more so for those under age 12 who need to be hospitalized for medical stabilization. I wrote this post (and part 2) to offer brief answers to some common questions about eating disorders because I receive many inquiries. None of the answers below are meant to be exhaustive. Websites for professional eating disorder organizations, books, and emerging research can be accessed for in depth explorations if you are interested. You’re also welcome to email me if you would like recommendations for further reading. For now though, I hope these short discussions provide some valuable information.
There are a variety of treatments that can work when it comes to healing an eating disorder. In general, eating disorders are about dieting, food rules, fear of weight gain, obsession with fitness, and scrutiny about body image, but they are also about coping with life stressors, relationships, and emotions. Eating disorders, which typically begin in early to late adolescence, are life threatening- having the second highest mortality rate among mental health problems.
A complete assessment is important: This is a crucial first step. If the assessment shows that you’re medically stable then you won’t need medical hospitalization.
The most effective care is a multidisciplinary approach: Eating disorders impact not just the body but the mind as well, interfering with how we think, behave, and feel. Treatment typically includes talk therapy, nutrition counseling, and medical management components—and sometimes medication is prescribed.
Numerous effective therapies may be helpful: Family-based therapy (FBT), cognitive behavioral therapy (CBT), and interpersonal therapy (IPT) are the most effective depending on the type and intensity of the eating disorder. Of these, CBT is the most common and is effective for all types of eating disorders. FBT is effective and recommended for children and adolescents with eating disorders, especially for anorexia nervosa. CBT, FBT, and IPT are evidence-based for binge eating disorder. A variety of other therapies may also be effective, depending on a person’s illness, situation, and their history.
Treatment options are tailored to the individual: That’s because recommended interventions can vary depending on an individual’s age, type of eating disorder, and the level of care that is needed for recovery. Most children, adolescents, and adults will start with outpatient therapy; however, in cases involving medical complications, hospitalization may be required.
Normalizing eating is primary: Eating regularly throughout the day without restricting, compensating, or binge eating is the primary goal of all treatment approaches. While CBT and FBT make this the explicit, IPT for binge eating disorder strengthens relationships as the path to healing. Most likely, you will start out with a structured approach to eating, then eventually move on to eating intuitively. Remember, even if recovery seems daunting, eating is natural. It can be natural again for you.
Improved coping is a target of treatment: Once your body and brain have been bathed in nutrition for long enough and you are no longer suffering from the impact of starvation or the dysregulation caused by purging, over exercising or binge eating, your mental energy can be turned toward other aspects of your wellbeing. Learning how to effectively manage stress, relationship difficulties, negative emotions and other triggers enables a person to eventually let go of the eating disorder behaviors. For some people, normalizing eating and better coping can be worked on simultaneously.
Eating disorders are biopsychosocial illnesses: Eating disorders have genetic, metabolic, psychological, and socio-cultural components. Therefore, complete healing incorporates a focus on all aspects of a person’s vulnerability to prevent relapse, after nutritional restoration is reached. Recovery is seen as a time when the mind and body are returned to a state of homeostasis and when food and eating disorder behaviors are no longer used to deal with life and living.
Eating disorders are life threatening and do not discriminate: They can affect any age, gender, race, socioeconomic status, or body size. Sadly, our culture is obsessed with weight and promotes dieting. Relatedly, 81% of 10 year old children are afraid of being fat and 9% of the U.S. population will have an eating disorder in their lifetime. Eating disorders are still underdiagnosed, especially in communities of color, in males, and in people who are not underweight.
Getting help early is key: Research shows that early intervention leads to better outcomes.
Full recovery is possible: Being free of an eating disorder offers you an opportunity to spend your mental and physical energy on value-driven goals and actions. Stay hopeful even if your motivation is low. We have treatments that work and professionals who are ready to help.

What is family-based therapy for eating disorders?
“Being recovered to me is when the person can accept his or her natural body size and shape, and no longer has a self-destructive or unnatural relationship with food or exercise. When you are recovered, food and weight take a proper perspective in your life, and what you weigh is not more important than who you are; in fact, actual numbers are of little or no importance at all. When recovered, you will not compromise your health or betray your soul to look a certain way, wear a certain size, or reach a certain number on a scale. When recovered, you do not use eating disorder behaviors to deal with, distract from, or cope with other problems.”
—Carolyn Costin
Family-based therapy (FBT) is a specialized form of family therapy combined with talk therapy that involves the child, parents or caregivers, and siblings. It has proven especially effective in treating children and adolescents with anorexia nervosa and other eating disorders.
FBT was developed because we recognize that families are strongly devoted to their children’s health and wellbeing. Rather than having a child or adolescent receive treatment in a center or with an individual therapist, then return home to confront the difficulty of eating meals and snacks without engaging in eating disorder behaviors, the family is trained to provide nutritional, behavioral, and emotional support at home until recovery is reached. The FBT approach respects that caregivers are uniquely powerful in their ability to leverage their love, insight, and devotion to motivate healing and support healthy actions when it comes to their child’s health. To give you a sense of how it works, below are some of the key components of FBT.
FBT has five core principles:
- It is agnostic: Therapists are not looking to blame anyone or to understand why the eating disorder happened.
- There’s a single focus: Having the child reach a state of weight, nutritional, and medical stabilization is the objective.
- Caregivers are in charge: Caretakers portion and supervise all meals and snacks.
- It is collaborative and non authoritarian: Parents are seen as the experts on their child, therapists are seen as the experts on eating disorders, and medical providers are seen as the experts on how the eating disorder impacts the body.
- The illness is externalized: The eating disorder is viewed as something a patient has, not who they are. For example, FBT would not characterize a person as “bulimic” but rather as “a person who has bulimia nervosa.” With FBT, the child or adolescent is viewed as someone with a life-threatening illness. The child, family, and professionals come together as one team to help fight off this externalized illness without shaming or blaming.
Beyond these principles, FBT seeks to intervene if perfectionism, interpersonal relationships, anxiety, OCD, depression or other problems are getting in the way of the recovery process.
Once the goal of nourishment is fully reached, the child or adolescent with the illness is allowed to portion meals and snacks until they are able to give themselves all that they need. Eventually, eating can be turned back over to the person who is recovering, supervision can be slowly withdrawn. The family, having been the central providers of support, motivation, and nutrition, are able to serve as an ongoing support system and offer backup in the future if there is a need to shore up relapse prevention.
At the conclusion of FBT, individual therapy may be recommended, offering the child or adolescent an opportunity to learn how to better cope with developmental concerns that may have emerged during FBT and to strengthen lingering vulnerabilities.
What is cognitive behavioral therapy for eating disorders?
“Cognitive therapy seeks to alleviate psychological stresses by correcting faulty conceptions and self-signals. By correcting erroneous beliefs we can lower excessive reactions.”
—Aaron Beck
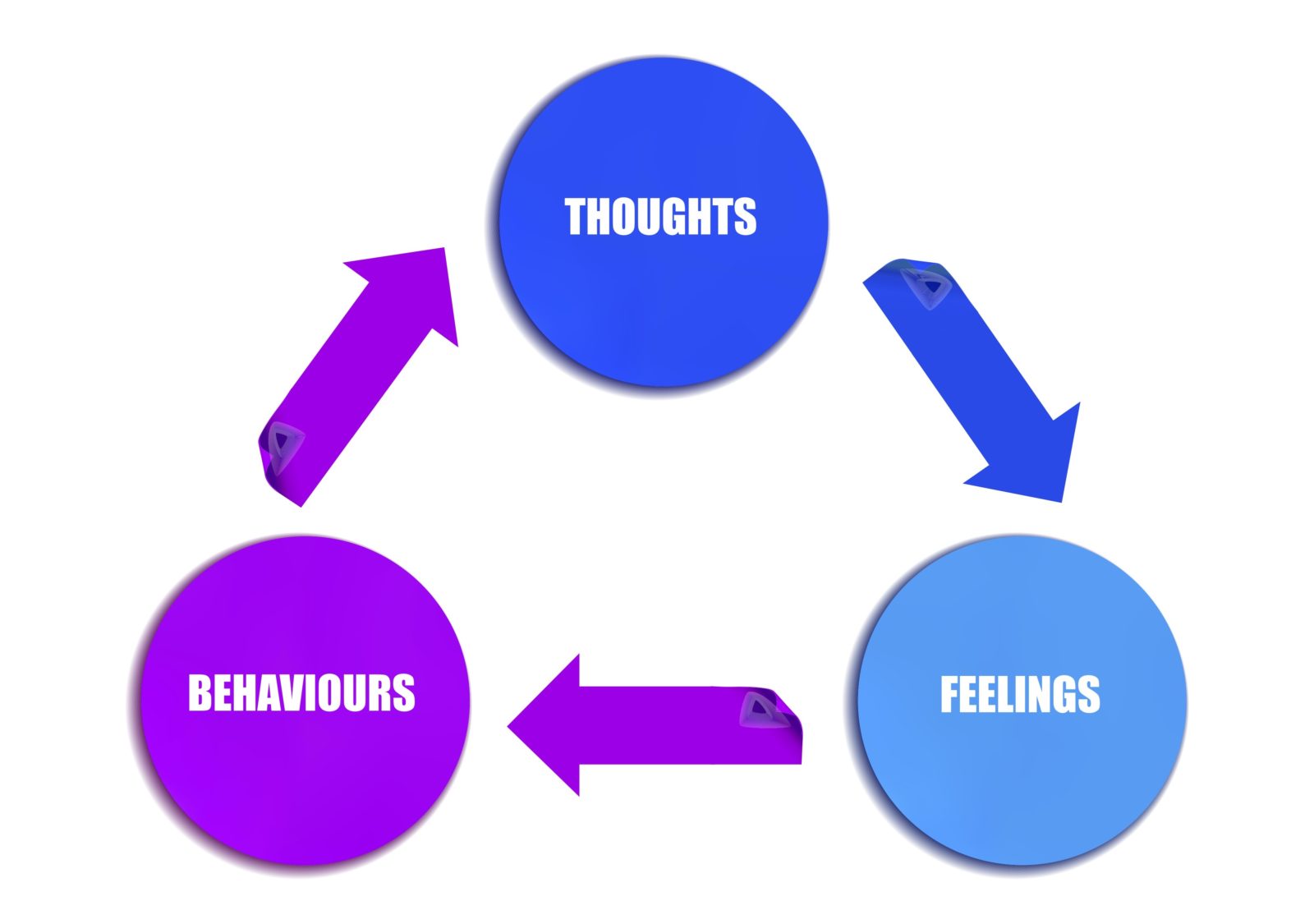
In terms of eating disorders, cognitive behavioral therapy (CBT) challenges the relationship among thoughts, behaviors, and emotions. Specifically, treatment focuses on the impact of overvaluation of weight, body shape, and control on behaviors and emotions. As with all treatments, many books have been written about CBT and its implementation. The goal here is to give you a feel for how it works so you can seek out more information if it gets you curious.
Challenges negative thoughts about weight, shape, size, and fitness: CBT helps people identify, evaluate, and change distressing thoughts and behaviors.
Develops more helpful coping in response to triggers: A variety of factors can lead to eating disorder behaviors – such as consistently eating in the absence of hunger, continuing to eat despite fullness, or restricting in the presence of hunger. CBT treatment helps an individual to identify the triggers that come before their eating disordered behaviors. That awareness opens up an opportunity for change, using experiments to try out new, healthy coping strategies.
Uses structured eating to normalize relationship to food: CBT allows an individual to think more realistically and more flexibly about weight and shape concerns that have been driving them, thereby reducing the likelihood of engaging in dieting, binge eating, purging, and other eating disorder behaviors. Clients are encouraged to not go longer than 3-4 hours between eating and to eat three meals and two to three snacks every day. By making eating more predictable, the mind and body can relax, reducing the physical and psychological results of starvation and the urge to engage in binge eating. Tolerating normal eating is tackled through tracking eating and reviewing food records in sessions.
Breaks the negative cycle: In CBT, helping an individual better understand their triggering thoughts related to an overconcern with shape and weight is key, because if left untreated those harmful thoughts can drive the onset and maintenance of serious negative cycles. For example, rigid beliefs about body shape can lead to cutting calories, which can then lead to malnutrition or binge eating.
Eating disorder thoughts are exhausting and distracting: In the past two decades of working with more than a thousand people with eating disorders, I have listened while many individuals have estimated that their thoughts about food, eating, calories, weight, fitness, and size had been taking up more than 90% of their thoughts when they began treatment. They felt physically exhausted and mentally trapped. But, with effective treatment, it doesn’t have to be this way. Your mind can be free.
Cognitive Behavioral Therapy (CBT) is the most frequently employed evidence-based treatment for helping with recovery from an eating disorder. The interventions aim to break the negative cognition-and-behavior cycle, targeting the unhelpful thoughts that start and maintain eating disorder behaviors. And, it works.
If you have an eating disorder, you don’t have to continue to suffer. What percentage of your day is spent thinking eating disorder thoughts? I know that you can find better ways to use your mental energy. Right now, imagine reaching full recovery. What would you do with all the time that the eating disorder no longer takes up?
All Blogs


